It is estimated that more than 2.5 million emergency department visits and 56,000 deaths each year are caused by traumatic brain injuries (TBI). Most TBIs are caused by falls, direct blows to the head, motor vehicle collisions, and blast injuries in war zones. In recent years, a lot of attention has been given to TBI and concussion that are sustained during sports such as football and hockey, and military service members returning from areas of conflict. All three of these activities expose participants to concussions and blows to the head over and over again. The problem with this is that although the symptoms of a mild TBI (mTBI) may not be concerning immediately, when the brain sustains additional injury, the problems compound. Reoccuring TBI, mTBI, and concussion can cause a variety of memory and personality changes, behavior and mental health problems, and long-term headaches, vision and hearing changes, and difficulty concentrating.
Trauma to the brain affects the brain in several ways. First, the actual injury to the brain tissue itself, caused by swelling and bruising of the brain tissue and bleeding within the surrounding area can cause a build-up of scar tissue of permanent death of the tissue affected. Additionally, axons and neurons that are the nerve fibers and wiring in the brain, are damaged, which leads to persistent, long-term problems. There have even been studies that link brain atrophy caused by TBI to Alzheimer’s disease later in life.
How Radiology is Used in the Diagnosis and Treatment of TBI
For mild concussions or TBI that occurs without loss of consciousness or persistent symptoms, diagnostic testing is generally limited to memory recall and concentration tests, and treatment is limited to resting the brain. For those TBIs that result in loss of consciousness, persistent symptoms — inability to focus, change in personality, vision or hearing changes, —; leaking of fluid from the ears; external damage such as bleeding, bruising, bone compromise, or exposed tissue, radiology is used to visualize the extent of the damage.
CT Scan
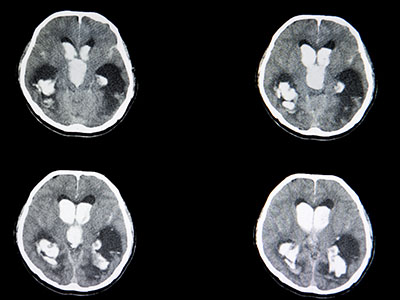
In the period immediately following the head trauma or TBI, computed tomography (CT) scan is used to visualize and diagnose acute, life-threatening problems. CT scans are a series of cross-sectional x-ray images that create a three-dimensional image. A CT scan can detect bleeding within and around the brain (hematoma), swelling (edema), skull fractures, and blood flow. These images can help direct emergency surgery or serve as baseline imaging for injuries that do not require surgical intervention. CT scans are quick and give a more complete picture than a traditional x-ray. Follow-up CT scans can be conducted once acute symptoms resolve to determine the extent of lasting damage and to ensure that damage has resolved.
MRI
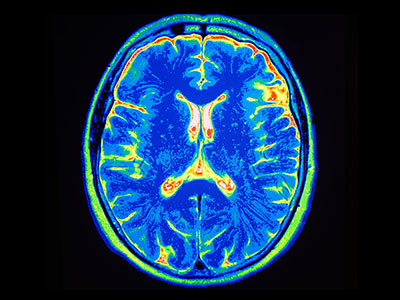
Magnetic resonance imaging (MRI) is a powerful tool that can detect microscopic injuries including damage to nerve fibers. MRI can also reveal very small bleeds (microhemorrhage), small bruises, and scarring (gliosis), that are not visible on a CT scan. MRI can also detect brain atrophy, which can be caused by recurrent TBI. Advanced NeuroQuant® imaging software technology can map the brain and measure volume compared to normal baselines.
If you require a CT scan or MRI to capture images of your brain following a TBI, trust the radiology experts at Touchstone Imaging. Our medical imaging centers feature state-of-the-art imaging equipment paired with experienced radiology technologists and the latest imaging software to provide high-quality images that help your physician make an accurate diagnosis and guide effective treatment plans. Visit us online to find out more information about our CT and MRI services and find a location near you.